
Bingo anyone? Environmental Justice, PFAS and COVID-19 Just Lined Up
Did anyone have on their 2020/2021 bingo card that PFAS could be related to increased likelihood of severe COVID-19 disease, reduced vaccine efficacy, and increased COVID-19 hospitalization and death rates among non-white populations? Bingo used to be fun …
The intersection of PFAS and COVID-19 is one of the latest environmental justice concerns facing disadvantaged communities today. Environmental justice seeks to provide the same level of protection to all people, regardless of race or socioeconomic status, from harm due to environmental and health hazards. Specifically, the US EPA defines environmental justice as, “the fair treatment and meaningful involvement of all people regardless of race, color, national origin or income, with respect to the development, implementation, and enforcement of environmental laws, regulations and policies.”
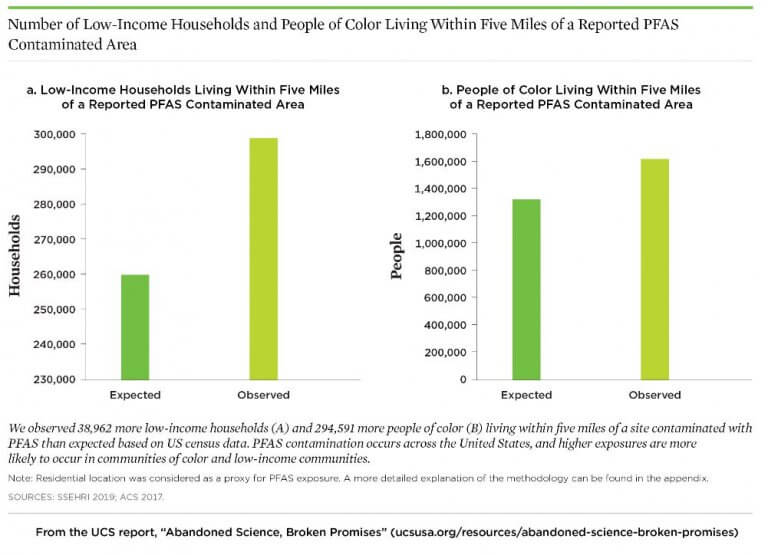
It is estimated that the drinking water of 110 million Americans may be contaminated with PFAS. Using census data, the Union of Concerned Scientists (UCS) found that low-income households and people of color are more likely to live near sites contaminated with PFAS.1
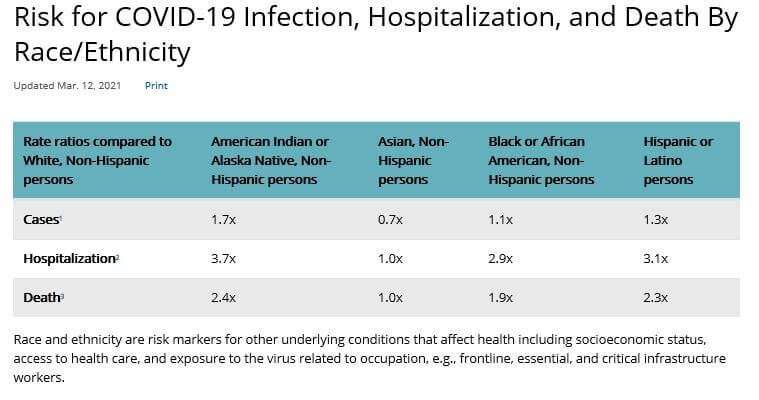
Additionally, the Centers for Disease Control and Prevention (CDC) found that the risk of hospitalization or death from COVID-19 for Black, Hispanic, or Indigenous populations was 2‑3× greater than White populations.2
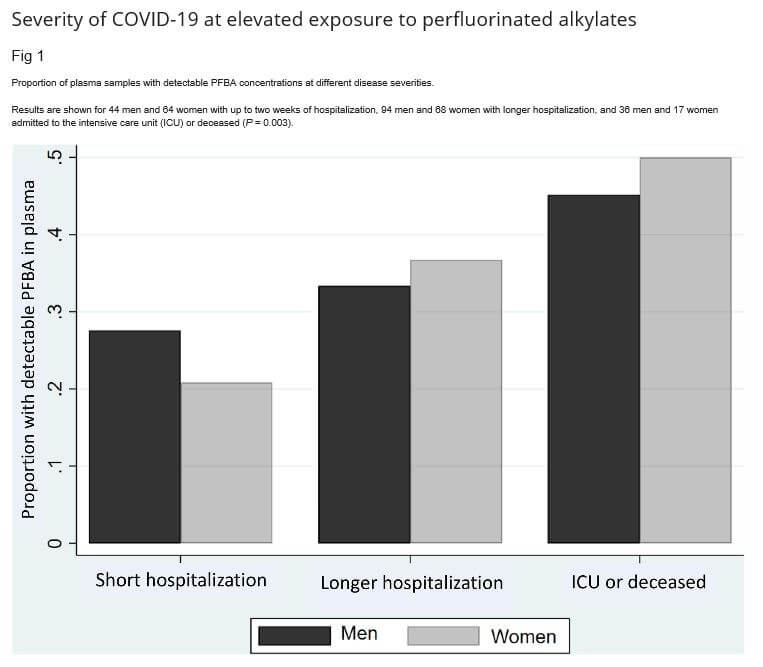
To evaluate the relationship and intersection of PFAS and COVID-19, several studies have been completed or are currently underway. In a recent Harvard University study conducted on Danish blood plasma samples, detections of pentafluorobenzoic acid (PFBA) in blood plasma were shown to be associated with more severe COVID-19 illness. As concentrations of PFBA increased, so did the likelihood of hospital ICU admission or death.3 PFBA has a relatively short half-life and is generally found in the blood in lower concentrations than other PFAS compounds, which made this finding surprising. However, other studies have shown that PFBA accumulates in the lungs and this may explain why it appears that higher levels of PFBA in the body leads to greater likelihood of severe COVID-19 illness.4
There is also a concern whether increased exposure to PFAS may impact vaccine efficacy. The Agency for Toxic Substances and Disease Registry (ATSDR) and the CDC recently commented that while more research is needed to fully understand how exposure to PFAS can affect an individual who becomes ill from COVD-19, there is evidence in both human and animal studies that show reduced antibody responses to vaccines in individuals with exposure to PFAS.
The ATSDR released the following statement, “CDC/ATSDR recognizes that exposure to high levels of PFAS may impact the immune system. There is evidence from human and animal studies that PFAS exposure may reduce antibody responses to vaccines (Grandjean et al., 2017, Looker et al., 2014), and may reduce infectious disease resistance (NTP, 2016). Because COVID-19 is a new public health concern, our knowledge of its impact on health is unclear. More research is needed to understand how PFAS exposure may affect illness from COVID-19.”5
The retired director of the National Institute for Environmental Health Sciences, Dr. Linda Birnbaum, stated, “we know (PFAS) do suppress the immune system. We know that if you have higher levels, you’re more likely to have that suppression happening. And we know that suppression of the immune system can be associated with decreased ability to mount a therapeutic response to vaccination.”6
A health study is underway by CDC and ATSDR to evaluate the intersection of PFAS exposure and COVID-19 in eight communities with elevated levels of PFAS. The study will measure PFAS concentrations in serum of healthcare personnel and first responders and their associated antibody response to COVID-19 as well as their symptoms, duration and treatment for COVID-19.
COVID-19 has shed a light on inequities in our society. Although more studies are needed to show whether there is a causal link between PFAS and COVID-19, we know enough today to ensure that vaccine distribution is equitable and make every effort to ramp up distribution in underserved communities. We are learning more about PFAS every day, and here at Environmental Standards, we are staying on top of the changing regulatory climate, method development, and ever-expanding PFAS compound lists.
References
- Desikan, Anita, Jacob Carter, Shea Kinser, and Gretchen Goldman. 2019. Abandoned Science, Broken Promises: How the Trump Administration’s Neglect of Science Is Leaving Marginalized Communities Further Behind. Cambridge, MA: Union of Concerned Scientists. October 23, 2019.
- Center for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization and Death by Race/Ethnicity. Updated March 12, 2021.
- Grandjean P, Timmermann CAG, Kruse M, Nielsen F, Vinholt PJ, Boding L, et al. Severity of COVID-19 at elevated exposure to perfluorinated alkylates. PLoS ONE 15(12): e0244815. https://doi.org/10.1371/journal.pone.0244815. December 31, 2020.
- Francisca Pérez, Martí Nadal, Alícia Navarro-Ortega, Francesc Fàbrega, José L. Domingo, Damià Barceló, Marinella Farré. Accumulation of perfluoroalkyl substances in human tissues, Environment International, Volume 59. Pages 354-362. ISSN 0160-4120. 2013.
- Agency for Toxic Substances and Disease Registry. What are the Health Effects of PFAS? Reviewed June 24, 2020.
- Ellison, Garrett. PFAS Exposure May Reduce COVID-19 Vaccine Potency, Experts Warn. MLive.com. https://www.mlive.com/public-interest/2020/12/pfas-exposure-may-reduce-covid-19-vaccine-potency-experts-warn.html


